Division of Cancer Information and Control
Introduction
We are conducting descriptive epidemiological studies using data from population-based cancer registries, hospital-based cancer registries, other medical sources, and various public entities focusing on health and medicine in Aichi Prefecture, Japan, and the world. In recent years, we have made a particular emphasis on spatial epidemiological analysis. We believe that our research can contribute to reducing the number of people who develop and die from cancer, and helping those who have cancer to receive treatment and live comfortably. In addition, through strong collaboration with the Division of Cancer Epidemiology and Prevention, we are accumulating evidence on how to improve preventive efforts and medical care.
Research topics
Overview of our research
The main purpose and focus of our research are as follows:
Descriptive epidemiologic studies of cancer incidence, mortality, and survival, focusing on improving the Aichi Prefectural Cancer Registry.
Since 1983, we have provided technical and statistical support to improve the accuracy of the Aichi Prefecture cancer registry operated by Aichi Prefecture. Furthermore, in April 2009, the “Office on Cancer Information Research” was established to strengthen support for the Aichi Cancer Registry and maximize the use of data. Even after the “nation cancer registration” was started in 2016, we continued to support the practice of cancer registration in Aichi Prefecture. Since April 2018, the “Office on Cancer Information Research” has been expanded to the “Division of Cancer Information and Control.” Our research has been improved using data from cancer registries in Aichi Prefecture, Japan and worldwide to characterize cancer incidence, mortality, and survival, specifying the numbers of people who are diagnosed with or die from cancer and who survive and are cured.
Population-based cancer registry
Population-based cancer registration is the gold standard for collecting information on cancer incidence in a defined population (Japan, Aichi Prefecture, etc.)
In Japan, the “National Cancer Registry” was started in January 2016 and is a nation-wide reliable cancer surveillance system, stated to be a key element in the Cancer Control Act of Japan.
In Aichi Prefecture, the Aichi Cancer Registry, which was started in 1962, has been incorporated into the National Cancer Registry. Information on cancer patients in Aichi Prefecture is summarized every year as a report on “cancer registration in Aichi prefecture.”
Descriptive epidemiology in cancer
Using data from the population-based cancer registry in Aichi, Japan and worldwide, we analyze the characteristics and trends of cancer incidence, mortality, and survival. In recent years, our additional focus has been spatial epidemiology. The descriptive results are useful for not only understanding cancer burden and monitoring cancer control but also identifying major areas in which cancer research should be conducted. A continued emphasis is on anonymized data.
We introduce some of the results of our studies.
Changes in survival of patients with non-small cell lung cancer in Japan: An interrupted time series study (TaniyamaY, Koyanagi YN, Ito H, et al. Cancer Science 2022 in press)
The epidermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKIs) gefitinib and erlotinib were approved for metastatic or relapsed non-small cell lung cancer (NSCLC) in Japan in 2002 and 2007, respectively. EGFR mutation testing was also approved in 2007. Although clinical trials showed efficacy in NSCLC patients harboring activating EGFR mutations, positive effects have only rarely been reported in real-world practice. We evaluated changes in survival in NSCLC patients following introduction of these agents and EGFR mutation testing by extracting cases from 1993 through 2011 from six prefectural population-based cancer registries in Japan. Relative survival (RS) was calculated by sex, histological subtype, and cancer stage. We conducted interrupted time series analysis to assess survival changes following introduction of EGFR-TKIs and EGFR mutation testing. A total of 120,068 patients with NSCLC were analyzed. One- and three-year RS gradually increased overall for men and women. For adenocarcinomas, among men, slopes of 1- and 3-year RS increased steeply in patients diagnosed from 2007 through 2011; among women, significant increments were seen in 1-year RS in those diagnosed in 2002 (4.55% [95% confidence interval: 1.76-7.33]) and 2007 (3.40% [1.27-5.52]) (Fig. 1).
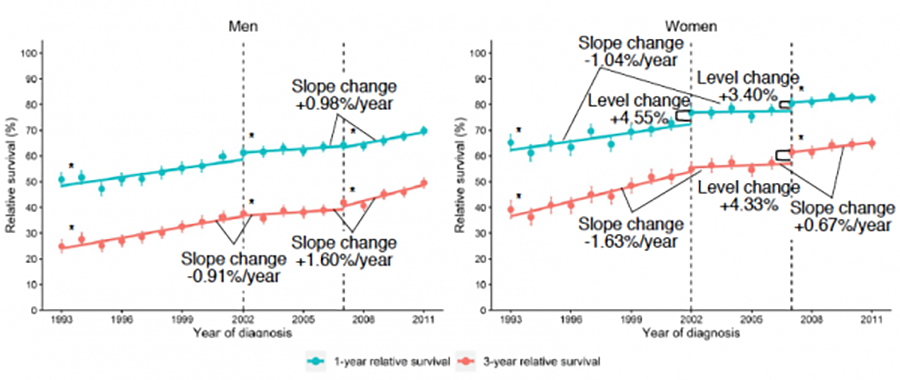
These significant increases were particularly obvious in women with advanced stage adenocarcinomas. Our results suggest that recent improvements in survival in men and women with adenocarcinoma are due at least partly to introduction of EGFR-TKIs into real-world practice, and to prescriptions based on appropriate patient selection following introduction of EGFR mutation testing into real-world practice in Japan.
Change in trend in mortality rate of multiple myeloma after introduction of novel agents: A population-based study (Usui Y, Ito H, Matsuo K, et al. Int J Cancer; 147:3102-3109, 2020)
Previously, the main treatment for multiple myeloma (MM) was cytotoxic chemotherapy, along with autologous stem-cell transplantation (ASCT), but survival benefit in the elderly was limited. More recently, clinical trials and practical experience have shown superior efficacy of novel agents . However, this improvement cannot be simply interpreted as a decline in mortality assessed as an important public health measure of progress against cancer. Here, we compared trends in mortality rates for MM in parallel with incidence rates in Japan and the U.S., using national mortality data and population-based cancer registry data in both countries from 1995 to 2015, during which 74 972 patients in Japan and 229 290 patients in the U.S. died of MM. Trends in mortality and incidence rates were characterized using joinpoint regression analysis. Despite upward trends in incidence, mortality rates showed a significant reduction after 2005 in Japan, with an annual percent change [APC (95% confidence interval)] of -2.5% (-2.9% to -2.1%), and after 2002 in the U.S., with an APC of -2.0% (-2.6% to -1.5%). In both countries, the change in mortality trend coincided with the introduction of the novel agents. Moreover, improvements in mortality were particularly large in patients aged 70 to 79 years, who are not eligible for ASCT. Our results indicate that the benefits of novel agents for MM are appreciable at the population level and provide encouragement for further development of novel agents for malignancies that can be widely applied.
Potential overtreatment among men aged 80 years and older with localized prostate cancer in Japan (Masaoka H, Ito H, Matsuo K, et al. Cancer Science; 108(8): 1673-1680, 2017)
Despite treatment guidelines recommending observation of men with low-risk prostate cancer with a life expectancy <10 years, most elderly patients choose active intervention, which may result in overtreatment. Because of the growing burden of prostate cancer among men aged ≥80 years (super-elderly men), accumulation of survival data for evaluating this possibility is imperative. A population-based cohort study was therefore conducted using cancer registry data from the Monitoring of Cancer Incidence in Japan project, which covers 47% of the Japanese population.
The subjects were men diagnosed with prostate cancer between 2006 and 2008 and the follow-up period was 5 years. We calculated 5-year relative survival rates among active treatment and observation groups after imputation for missing values.
Of the 48,782 patients with prostate cancer included in the analysis, 15.1% were super-elderly men. Among men aged ≥80 years, the 5-year relative survival rates for regional and distant cancer were 90.7% and 50.4%, respectively. In contrast, for localized cancer, patients in all age categories had 5-year relative survival rates >100% (Fig. 2).
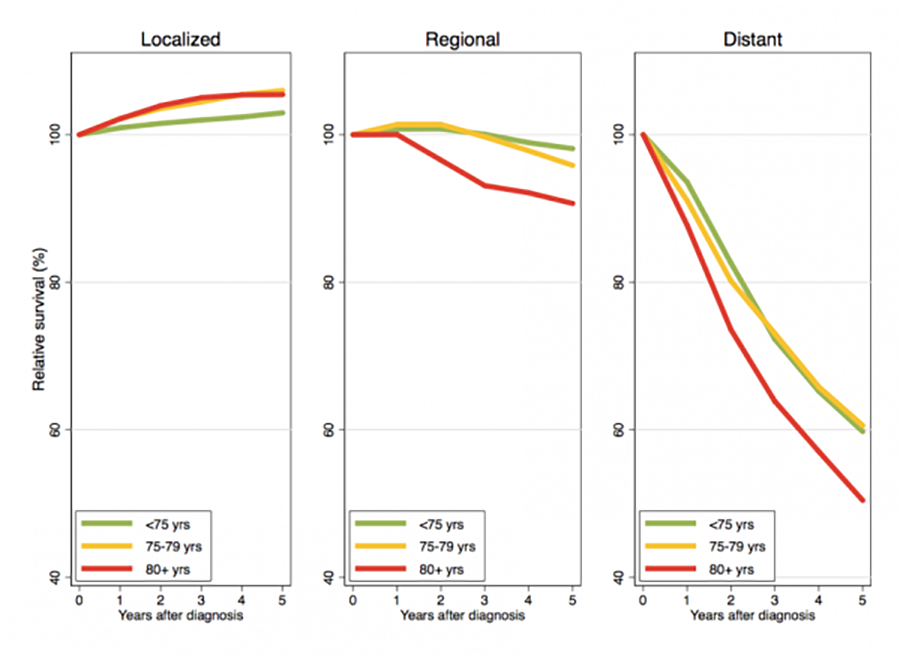
The 5-year relative survival rates of super-elderly men aged ≥80 years with localized cancer were 105.9% and 104.1% for the active treatment and observation groups, respectively (Fig. 3). For well- and moderately differentiated localized cancer, the 5-year relative survival rates were >100% in all age categories. For poorly differentiated localized cancer, the 5-year relative survival rate was near or > 100% among men aged ≥75 years, whereas men aged <75 years had a slightly lower 5-year relative survival rate without active treatment, albeit without statistical significance.
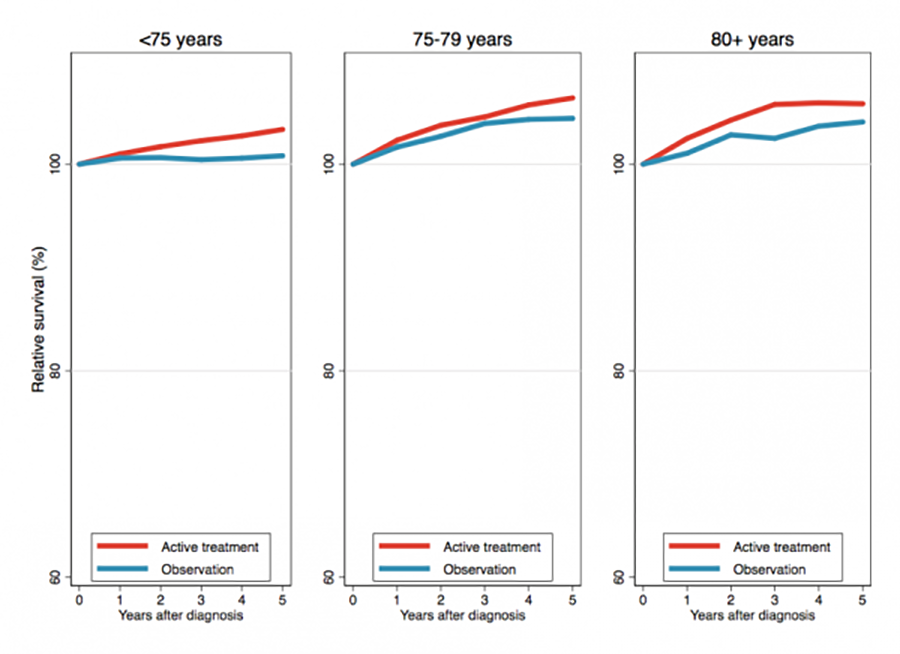
In conclusion, super-elderly men with localized prostate cancer may live for as long as the general population of the same age regardless of tumor grade, even if they do receive active intervention. More than half of super-elderly men with localized prostate cancer may be overtreated in Japan.
Members
Publications
Original articles
- Taniyama Y, Oze I, Koyanagi YN, Kawakatsu Y, Ito Y, Matsuda T, Matsuo K, Mitsudomi T, Ito H. Changes in survival of patients with non-small cell lung cancer in Japan: An interrupted time series study. Cancer Sci. 2022 Nov 11.
- Koyanagi YN, Oze I, Kasugai Y, Kawakatsu Y, Taniyama Y, Hara K, Shimizu Y, Imoto I, Ito H, Matsuo K. New insights into the genetic contribution of ALDH2 rs671 in pancreatic carcinogenesis: Evaluation by mediation analysis. Cancer Sci. 2022 Apr;113(4):1441-1450.
- Kawakita D, Oze I, Iwasaki S, Matsuda T, Matsuo K, Ito H. Trends in the incidence of head and neck cancer by subsite between 1993 and 2015 in Japan. Cancer Med. 2022 Mar;11(6):1553-1560.
- Masuda T, Ito H, Hirata J, Sakaue S, Ueda Y, Kimura T, Takeuchi F, Murakami Y, Matsuda K, Matsuo K, Okada Y. Fine Mapping of the Major Histocompatibility Complex Region and Association of the HLA-B*52:01 Allele With Cervical Cancer in Japanese Women. JAMA Netw Open. 2020 Oct 1;3(10):e2023248.
- Ishikura N, Ito H, Oze I, Koyanagi YN, Kasugai Y, Taniyama Y, Kawakatsu Y, Tanaka T, Ito S, Tajika M, Shimizu Y, Niwa Y, Matsuo K. Risk Prediction for Gastric Cancer Using GWAS-Identified Polymorphisms Helicobacter pylori Infection and Lifestyle-Related Risk Factors in a Japanese Population. Cancers (Basel). 2021 Nov 3;13(21):5525.
- Kawakatsu Y, Koyanagi YN, Oze I, Kasugai Y, Morioka H, Yamaguchi R, Ito H, Matsuo K. Association between Socioeconomic Status and Digestive Tract Cancers: A Case-Control Study. Cancers (Basel). 2020 Nov 4;12(11):3258.
- Shimatani K, Ito H, Matsuo K, Tajima K, Takezaki T. Cumulative cigarette tar exposure and lung cancer risk among Japanese smokers. Jpn J Clin Oncol. 2020 Sep 5;50(9):1009-1017.
- Usui Y, Ito H, Koyanagi Y, Shibata A, Matsuda T, Katanoda K, Maeda Y, Matsuo K. Changing trend in mortality rate of multiple myeloma after introduction of novel agents: A population-based study. Int J Cancer. 2020 Dec 1;147(11):3102-3109.
- Koyanagi YN, Suzuki E, Imoto I, Kasugai Y, Oze I, Ugai T, Iwase M, Usui Y, Kawakatsu Y, Sawabe M, Hirayama Y, Tanaka T, Abe T, Ito S, Komori K, Hanai N, Tajika M, Shimizu Y, Niwa Y, Ito H, Matsuo K. Across-Site Differences in the Mechanism of Alcohol-Induced Digestive Tract Carcinogenesis: An Evaluation by Mediation Analysis. Cancer Res. 2020 Apr 1;80(7):1601-1610.
- Ugai T, Ito H, Oze I, Saito E, Rahman MS, Boffetta P, Gupta PC, Sawada N, Tamakoshi A, Shu XO, Koh WP, Gao YT, Sadakane A, Tsuji I, Park SK, Nagata C, You SL, Pednekar MS, Tsugane S, Cai H, Yuan JM, Xiang YB, Ozasa K, Tomata Y, Kanemura S, Sugawara Y, Wada K, Chen CJ, Yoo KY, Chia KS, Ahsan H, Zheng W, Inoue M, Kang D, Potter J, Matsuo K. Association of BMI, Smoking, and Alcohol with Multiple Myeloma Mortality in Asians: A Pooled Analysis of More than 800,000 Participants in the Asia Cohort Consortium. Cancer Epidemiol Biomarkers Prev. 2019 Nov;28(11):1861-1867.
- Nakagawa-Senda H, Hori M, Matsuda T, Ito H. Prognostic impact of tumor location in colon cancer: the Monitoring of Cancer Incidence in Japan (MCIJ) project. BMC Cancer. 2019 May 9;19(1):431.
- Koyanagi YN, Ito H, Matsuo K, Sugawara Y, Hidaka A, Sawada N, Wada K, Nagata C, Tamakoshi A, Lin Y, Takeuchi T, Kitamura Y, Utada M, Sadakane A, Mizoue T, Naito M, Tanaka K, Shimazu T, Tsugane S, Inoue M; Research Group for the Development and Evaluation of Cancer Prevention Strategies in Japan. Smoking and Pancreatic Cancer Incidence: A Pooled Analysis of 10 Population-Based Cohort Studies in Japan. Cancer Epidemiol Biomarkers Prev. 2019 Aug;28(8):1370-1378.
- Ishiguro J, Ito H, Tsukamoto M, Iwata H, Nakagawa H, Matsuo K. A functional single nucleotide polymorphism in ABCC11, rs17822931, is associated with the risk of breast cancer in Japanese. Carcinogenesis. 2019 Jun 10;40(4):537-543.
- Kotani H, Ito H, Kuwahara K, Kuzushima K, Iwata H, Tsunoda N, Nagino M, Matsuo K. Impact of germinal center-associated nuclear protein polymorphisms on breast cancer risk and prognosis in a Japanese population. Breast Cancer. 2019 Sep;26(5):562-572.
- Inoue S, Ito H, Hosono S, Hori M, Matsuda T, Mizuno M, Kato K, Matsuo K. Net Survival of Elderly Patients with Gynecological Cancer Aged Over 75 Years in 2006-2008. Asian Pac J Cancer Prev. 2019 Feb 26;20(2):437-442.
- Yoshimura A, Ito H, Nishino Y, Hattori M, Matsuda T, Miyashiro I, Nakayama T, Iwata H, Matsuo K, Tanaka H, Ito Y. Recent Improvement in the Long-term Survival of Breast Cancer Patients by Age and Stage in Japan. J Epidemiol. 2018 Oct 5;28(10):420-427.
- Inoue S, Hosono S, Ito H, Oze I, Nishino Y, Hattori M, Matsuda T, Miyashiro I, Nakayama T, Mizuno M, Matsuo K, Kato K, Tanaka H, Ito Y; J-CANSIS Research Group. Improvement in 5-Year Relative Survival in Cancer of the Corpus Uteri From 1993-2000 to 2001-2006 in Japan. J Epidemiol. 2018 Feb 5;28(2):75-80.
- Koyanagi YN, Matsuo K, Ito H, Tamakoshi A, Sugawara Y, Hidaka A, Wada K, Oze I, Kitamura Y, Liu R, Mizoue T, Sawada N, Nagata C, Wakai K, Nakayama T, Sadakane A, Tanaka K, Inoue M, Tsugane S, Sasazuki S. Body-Mass Index and Pancreatic Cancer Incidence: A Pooled Analysis of Nine Population-Based Cohort Studies With More Than 340,000 Japanese Subjects. J Epidemiol. 2018 May 5;28(5):245-252.
- Nakagawa-Senda H, Yamaguchi M, Matsuda T, Koide K, Kondo Y, Tanaka H, Ito H. Cancer Prevalence in Aichi, Japan for 2012: Estimates Based on Incidence and Survival Data from Population-Based Cancer Registry. Asian Pac J Cancer Prev. 2017 Aug 27;18(8):2151-2156.
- Masaoka H, Ito H, Yokomizo A, Eto M, Matsuo K. Potential overtreatment among men aged 80 years and older with localized prostate cancer in Japan. Cancer Sci. 2017 Aug;108(8):1673-1680.
- Nakagawa-Senda H, Ito H, Hosono S, Oze I, Tanaka H, Matsuo K. Coffee consumption and the risk of colorectal cancer by anatomical subsite in Japan: Results from the HERPACC studies. Int J Cancer. 2017 Jul 15;141(2):298-308.
- Koyanagi YN, Ito H, Oze I, Hosono S, Tanaka H, Abe T, Shimizu Y, Hasegawa Y, Matsuo K. Development of a prediction model and estimation of cumulative risk for upper aerodigestive tract cancer on the basis of the aldehyde dehydrogenase 2 genotype and alcohol consumption in a Japanese population. Eur J Cancer Prev. 2017 Jan;26(1):38-47.
- Koyanagi YN, Matsuo K, Ito H, Wakai K, Nagata C, Nakayama T, Sadakane A, Tanaka K, Tamakoshi A, Sugawara Y, Mizoue T, Sawada N, Inoue M, Tsugane S, Sasazuki S; Research Group for the Development and Evaluation of Cancer Prevention Strategies in Japan, Sasazuki S, Tsugane S, Inoue M, Iwasaki M, Otani T, Sawada N, Shimazu T, Yamaji T, Tsuji I, Tsubono Y, Nishino Y, Tamakoshi A, Matsuo K, Ito H, Wakai K, Nagata C, Mizoue T, Tanaka K, Nakayama T, Sadakane A; Research Group for the Development and Evaluation of Cancer Prevention Strategies in Japan. Cigarette smoking and the risk of head and neck cancer in the Japanese population: a systematic review and meta-analysis. Jpn J Clin Oncol. 2016 Jun;46(6):580-95.
- Nakagawa H, Ito H, Hosono S, Oze I, Mikami H, Hattori M, Nishino Y, Sugiyama H, Nakata K, Tanaka H. Changes in trends in colorectal cancer incidence rate by anatomic site between 1978 and 2004 in Japan. Eur J Cancer Prev. 2017 Jul;26(4):269-276.
- Ito H, Matsuo K. Molecular epidemiology, and possible real-world applications in breast cancer. Breast Cancer. 2016 Jan;23(1):33-38.
- Chihara D, Ito H, Izutsu K, Hattori M, Nishino Y, Ioka A, Matsuda T, Ito Y. Advance and stagnation in the treatment of patients with lymphoma and myeloma: Analysis using population-based cancer registry data in Japan from 1993 to 2006. Int J Cancer. 2015 Sep 1;137(5):1217-23.
- Ito Y, Miyashiro I, Ito H, Hosono S, Chihara D, Nakata-Yamada K, Nakayama M, Matsuzaka M, Hattori M, Sugiyama H, Oze I, Tanaka R, Nomura E, Nishino Y, Matsuda T, Ioka A, Tsukuma H, Nakayama T; J-CANSIS Research Group. Long-term survival and conditional survival of cancer patients in Japan using population-based cancer registry data. Cancer Sci. 2014 Nov;105(11):1480-6.
- Chihara D, Ito H, Katanoda K, Shibata A, Matsuda T, Sobue T, Matsuo K. Incidence of myelodysplastic syndrome in Japan. J Epidemiol. 2014;24(6):469-73.
- Fukumoto K, Ito H, Matsuo K, Tanaka H, Yokoi K, Tajima K, Takezaki T. Cigarette smoke inhalation and risk of lung cancer: a case-control study in a large Japanese population. Eur J Cancer Prev. 2015 May;24(3):195-200.
- Chihara D, Ito H, Matsuda T, Shibata A, Katsumi A, Nakamura S, Tomotaka S, Morton LM, Weisenburger DD, Matsuo K. Differences in incidence and trends of haematological malignancies in Japan and the United States. Br J Haematol. 2014 Feb;164(4):536-45.
- Ito H, Gallus S, Hosono S, Oze I, Fukumoto K, Yatabe Y, Hida T, Mitsudomi T, Negri E, Yokoi K, Tajima K, La Vecchia C, Tanaka H, Matsuo K. Time to first cigarette and lung cancer risk in Japan. Ann Oncol. 2013 Nov;24(11):2870-5.
- Chihara D, Ito H, Matsuda T, Katanoda K, Shibata A, Saika K, Sobue T, Matsuo K. Decreasing trend in mortality of chronic myelogenous leukemia patients after introduction of imatinib in Japan and the U.S. Oncologist. 2012;17(12):1547-50.
- Chihara D, Ito H, Katanoda K, Shibata A, Matsuda T, Tajima K, Sobue T, Matsuo K. Increase in incidence of adult T-cell leukemia/lymphoma in non-endemic areas of Japan and the United States. Cancer Sci. 2012 Oct;103(10):1857-60.
- Ito H, McKay JD, Hosono S, Hida T, Yatabe Y, Mitsudomi T, Brennan P, Tanaka H, Matsuo K. Association between a genome-wide association study-identified locus and the risk of lung cancer in Japanese population. J Thorac Oncol. 2012 May;7(5):790-8.
- Sueta A, Ito H, Kawase T, Hirose K, Hosono S, Yatabe Y, Tajima K, Tanaka H, Iwata H, Iwase H, Matsuo K. A genetic risk predictor for breast cancer using a combination of low-penetrance polymorphisms in a Japanese population. Breast Cancer Res Treat. 2012 Apr;132(2):711-21.
- Ito H, Matsuo K, Tanaka H, Koestler DC, Ombao H, Fulton J, Shibata A, Fujita M, Sugiyama H, Soda M, Sobue T, Mor V. Nonfilter and filter cigarette consumption and the incidence of lung cancer by histological type in Japan and the United States: analysis of 30-year data from population-based cancer registries. Int J Cancer. 2011 Apr 15;128(8):1918-28.
- Ito H, Matsuo K, Wakai K, Saito T, Kumimoto H, Okuma K, Tajima K, Hamajima N. An intervention study of smoking cessation with feedback on genetic cancer susceptibility in Japan. Prev Med. 2006 Feb;42(2):102-8.
- Ito H, Matsuo K, Hamajima N, Okuma K, Saito T, Tajima K. Significant association of interleukin 8 -251T/A polymorphism with smoking behavior in a Japanese population. J Hum Genet. 2005;50(11):567-73.
- Ito H, Matsuo K, Hamajima N, Mitsudomi T, Sugiura T, Saito T, Yasue T, Lee KM, Kang D, Yoo KY, Sato S, Ueda R, Tajima K. Gene-environment interactions between the smoking habit and polymorphisms in the DNA repair genes, APE1 Asp148Glu and XRCC1 Arg399Gln, in Japanese lung cancer risk. Carcinogenesis. 2004 Aug;25(8):1395-401.
- Ito H, Hamajima N, Matsuo K, Okuma K, Sato S, Ueda R, Tajima K. Monoamine oxidase polymorphisms and smoking behaviour in Japanese. Pharmacogenetics. 2003 Feb;13(2):73-9.
- Ito H, Hamajima N, Takezaki T, Matsuo K, Tajima K, Hatooka S, Mitsudomi T, Suyama M, Sato S, Ueda R. A limited association of OGG1 Ser326Cys polymorphism for adenocarcinoma of the lung. J Epidemiol. 2002 May;12(3):258-65.
Education & Training
Building on broad experience and expertise, in collaboration with the staff of our research groups, the Division of Cancer Information & Control, Division of Cancer Epidemiology & Prevention, and Division of Molecular Genetics, we are offering training on descriptive through analytical approaches. Postdoctoral positions are available for highly motivated candidates with an appropriate background. Postdoctoral Fellows are eligible salary, health insurance, and VISA support. Informal inquiries can be sent to Hidemi Ito at hidemi@aichi-cc.jp. Additionally, the division is a part of Nagoya University Graduate School of Medicine. Foreign graduate students are welcome to study in our programs, including those who are supported by Japanese Government Monbusho (MEXT) scholarships.